Robots used to train carers, sleep-monitoring sensors, and pain-detecting apps – could these innovations shape the future of caregiving?
With the UK’s ageing population on the rise, the care sector is turning more to technology and AI to meet growing demands.
However, experts caution against depending too heavily on AI for care.
“AI can support, but it can’t replace the human touch,” says Dr Caroline Green from the University of Oxford.

Dr Caroline Green wants to see investment in people as well as AI
Dr. Green, who leads research at the Institute for Ethics in AI, shared her views during the AI in Social Care Summit at Oxford University in March.
She warned that AI systems may carry biases that could worsen discrimination and reinforce stereotypes. She also acknowledged public concerns over data privacy when using such technologies.
“There’s currently no formal government policy guiding the use of AI in social care,” she noted.
Dr. Green added, “Whether AI benefits those needing care depends on how future policies develop. It’s about whether individuals will still have choices—such as opting out of AI in their care—and whether AI will end up replacing human interaction in support services.
“We must tread carefully to ensure people’s future options remain open and that social care doesn’t lose its human element.”
Fall reduction
Thomas Tredinnick, head of AllyCares, oversees a system that uses sensors to monitor care home residents’ rooms during the night, listening for unusual sounds or activity.
When something out of the ordinary is detected, an audio clip is sent to carers on duty, allowing them to respond as needed.
Speaking from Oaklands Rest Home in Southampton, where the technology is in use, Mr. Tredinnick explained that it reduces the need for routine nighttime checks, helping residents sleep more peacefully.
“This allows care staff to focus on those who truly need attention,” he said.

Christine Herbert said she was initially worried when she heard her mother was being “monitored” by AI
Mr. Tredinnick believes the technology has helped reduce avoidable health issues that might otherwise lead to hospital visits by detecting early signs of problems such as falls or chest infections.
Christine Herbert shared that her 99-year-old mother, Betty, is among those being monitored by the system.
Initially, she was hesitant about the use of AI, likening it to a “baby monitor.”
“When Mum first moved in, I asked for regular checks because I was worried,” she said.
However, Mrs. Herbert said her concerns eased after the care home showed her detailed data proving that her mother was being monitored effectively without being disturbed at night.
App for pain
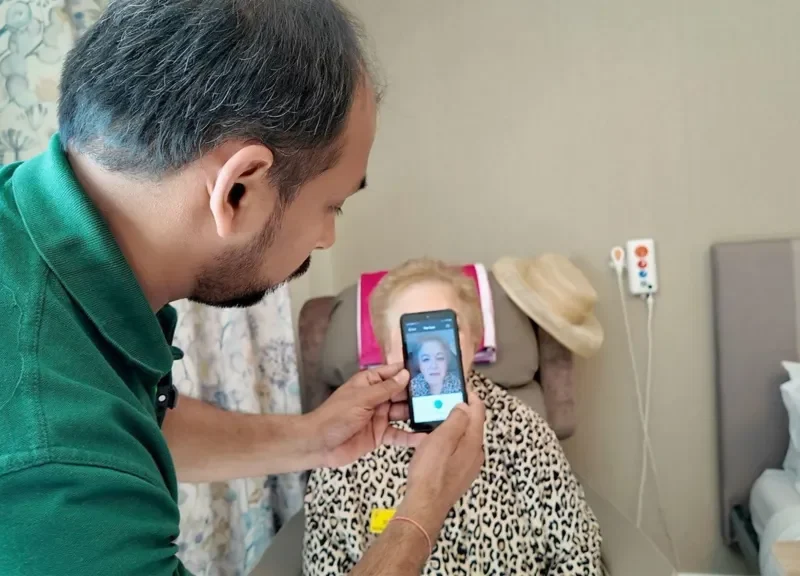
At Elmbrook Court care home in Wantage, Oxfordshire, staff are using AI to help detect pain in residents.
Deputy manager Aislinn Mullee explained, “It can be challenging to recognise pain in residents who are non-verbal.”
Carers use a smartphone app called Painchek, which scans a resident’s face for signs of pain, combines it with a short questionnaire, and generates an instant percentage score indicating the person’s pain level.
Ms. Mullee said the tool has made a “huge difference” and has been used alongside local GPs to determine appropriate pain relief.
She also mentioned it has helped reassure families that loved ones receiving end-of-life care are not in discomfort.
To protect privacy, she stressed that all data is password-protected and accessible only to care home staff.
Robot training
At the University of Oxford’s Robotics Institute, researchers are exploring how AI could assist in training future carers.
Dr. Marco Pontin, a Postdoctoral Research Assistant, is part of the team behind a robot designed to respond to human touch.
The robot can be programmed to simulate pain in specific areas and will physically flinch if a carer applies too much pressure to a sensitive spot.
It’s set to be tested with occupational therapy students at Oxford Brookes University as part of their training.

Robots will be used in the training of carers in Oxford
Dr. Pontin explained that the team aims to develop the robot into a “digital twin” of real-life patients.
By mirroring a patient’s specific medical conditions, the robot allows carers to simulate real-world scenarios and practice responses with a robotic stand-in.
“With an ageing population, it’s becoming more difficult to be present for every patient,” he said. “A digital twin could help occupational therapists monitor and understand their patients’ needs remotely.”
Care challenges
People in the UK are living longer, with around 12 million individuals aged 67 or older—a number expected to reach 13.7 million by 2032.
According to a March report from the House of Commons Library, local councils in England spent £23.3 billion on adult social care in 2023/24, making it the second-largest area of council expenditure after education.
The sector also faces staffing challenges, heavily depending on international workers. Home Office data revealed that 27,000 visas were granted for health and social care roles in the year ending December 2024—an 81% drop compared to the previous year. This follows a spike in numbers after temporary visa rule changes.
“We currently rely on migrant workers to sustain the social care system,” said Lee-Ann Fenge, Professor of Social Care at Bournemouth University.
She cautioned against viewing technology as a solution to workforce shortages. “It should be a tool that supports existing care practices,” she said.
Professor Fenge also emphasized the importance of addressing ethical concerns around surveillance and data use in care. “We must equip people to protect themselves. It’s not just about embracing AI—we need to weigh both its potential and its risks.”
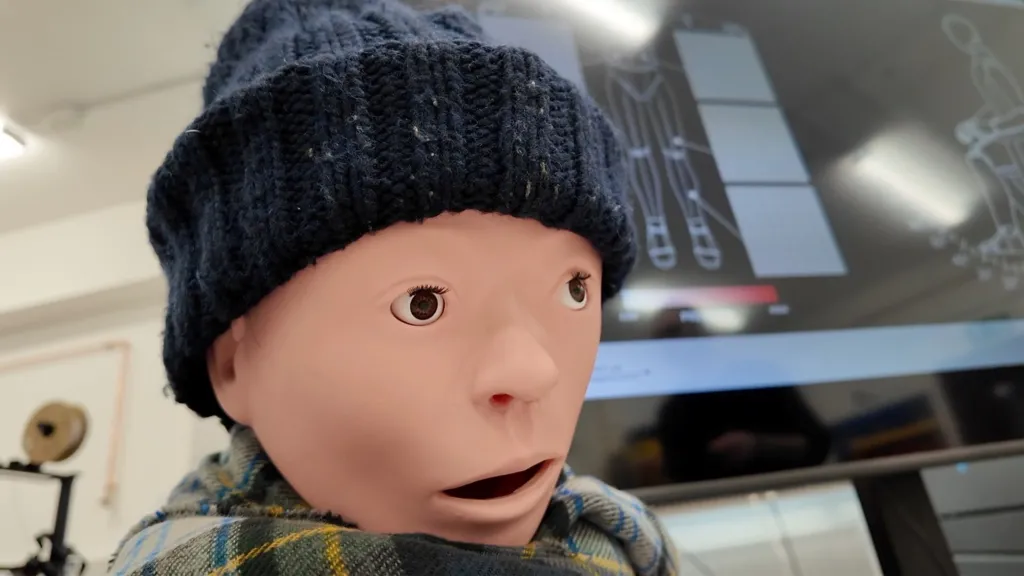
Dr. Pontin stated that the team aims to develop the robot into a “digital twin” that replicates real-life patients.
In February, both the UK and US governments declined to sign an international AI declaration in Paris that emphasized an “open,” “inclusive,” and “ethical” approach to AI development.
This decision came shortly after the UK government announced in March that it would adopt a “test and learn” approach to AI funding in the public sector to encourage innovation.
When speaking with Dr. Caroline Green again, she continued to advocate for a cautious approach to AI.
“AI can assist with administrative tasks and some operational aspects of care, but it cannot replace the human touch,” she stated.
She warned that there is a risk of AI being seen as a cure-all for the significant challenges in social care, such as staff shortages and the increasing demand driven by an ageing population.
“We need to ensure we don’t just invest in AI to replace caregiving. We must continue to invest in people and professionals who will provide the care,” she emphasized.
A spokesperson from the Department of Health and Social Care (DHSC) responded, “We are committed to using cutting-edge technology to transform social care. We’re already seeing promising advancements, such as AI-powered fall detection systems that enable earlier interventions, and tools that automate paperwork, allowing staff to focus more on direct care.”
They added, “Leveraging AI in social care is a key element of our 10-Year Health Plan, which aims to shift from treating illness to preventing it, from hospital-based care to community care, and from analogue to digital solutions.”