This is the fifth article in a six-part series exploring how AI is transforming medical research and healthcare treatments.
Securing a GP appointment in the UK is often challenging, and even when successful, doctors’ increasing workloads can result in shorter consultations than ideal for both parties.
Dr. Deepali Misra-Sharp, a GP partner in Birmingham, has turned to AI to ease her administrative burden and dedicate more attention to patients. About four months ago, she began using Heidi Health, a free AI-powered medical transcription tool that records and transcribes patient appointments, significantly improving her workflow.
“Typically, I’m writing notes during consultations, which detracts from the interaction,” she explains. “Now, I can fully engage with the patient, maintaining eye contact and listening actively, making the consultation more meaningful.”
The tool has reduced her workload, saving “two to three minutes per consultation, or more.” It also lowers the risk of errors or omissions in her notes.
With GP workloads increasing, the strain on the profession is evident. According to the British Medical Association (BMA), each full-time GP now manages an average of 2,273 patients—a 17% rise since 2015.
AI could be a game-changer in alleviating this pressure. A 2019 report by Health Education England suggested that even saving one minute per patient through AI technology could free up 5.7 million hours of GP time. Similarly, a 2020 Oxford University study found that 44% of administrative tasks in General Practice could be mostly or entirely automated, allowing more time for patient care.

Lars Maaloe (left) and Andreas Cleve co-founders of Danish medical AI firm Corti
Corti, a Danish company, is leveraging AI to transform healthcare consultations by providing tools that enhance efficiency and support clinical decisions. Their AI system listens to patient consultations, whether over the phone or in person, and assists by suggesting follow-up questions, treatment options, and automating note-taking.
Currently, Corti’s technology processes approximately 150,000 patient interactions daily across hospitals, GP practices, and healthcare institutions in Europe and the US, amounting to about 100 million consultations annually.
“The goal is for physicians to spend more time directly engaging with patients,” explains Lars Maaløe, Corti’s co-founder and CTO. The AI draws on its database of previous conversations to suggest relevant questions. “For instance, it might recognize that in 10,000 similar cases, most doctors asked a specific question that hasn’t yet been addressed,” says Maaløe.
Additionally, the AI can access a patient’s medical history to offer tailored prompts. “It could remind the doctor to ask if the patient is still experiencing knee pain,” he adds.
However, the idea of AI listening in on consultations raises privacy concerns. Maaløe assures that “the data stays within the system” and emphasizes the importance of informing patients. “If a patient objects, the doctor cannot record. However, most patients appreciate the improved documentation.”
Dr. Misra-Sharp, who uses AI for note-taking, ensures her patients are informed about the technology. “So far, no one has raised concerns. If they did, I’d respect their wishes and not use it.”
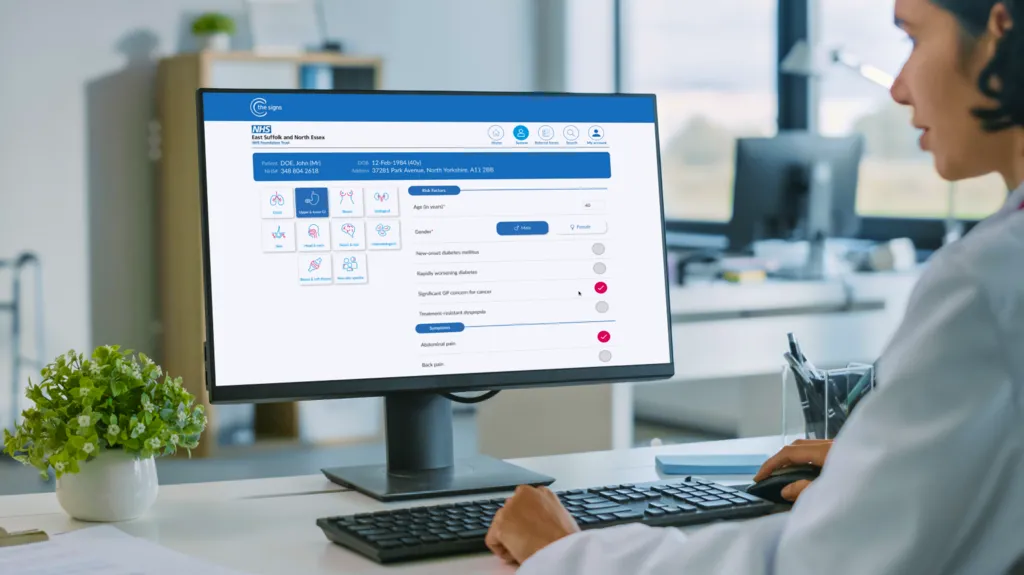
C the Signs software is used to analyse a patients medical record
Currently, 1,400 GP practices across England utilize C the Signs, an AI-powered platform designed to analyze medical records, identify cancer-related symptoms, and recommend next steps.
“It can quickly assess symptoms like cough, cold, or bloating and identify relevant information from a patient’s medical history within a minute,” explains Dr. Bea Bakshi, C the Signs CEO, co-founder, and practicing GP. Trained on medical research, the AI suggests potential risks and actions. For instance, it might flag a patient as being at risk for pancreatic cancer and recommend a scan, leaving the referral decision to the GP.
To date, the platform has facilitated over 400,000 cancer risk assessments, identifying more than 30,000 cases across 50+ cancer types.
A British Medical Association (BMA) AI report highlights that AI is expected to transform healthcare by automating routine tasks and enhancing efficiency, not replacing medical professionals. However, Dr. Katie Bramall-Stainer, chair of the BMA’s General Practice Committee, stresses the need for caution. “AI can revolutionize NHS care but must be implemented safely to avoid harm,” she warns, citing potential issues like bias, errors, and patient privacy risks.
Alison Dennis, co-head of Taylor Wessing’s life sciences team, underscores that only AI tools trained on validated datasets should be used in clinical practice. She emphasizes that regulatory oversight and secure data handling are crucial.
Despite these challenges, GPs like Dr. Misra-Sharp report significant benefits. “AI has allowed me to focus on patients, making consultations enjoyable again instead of a race against time,” she shares.











